For new readers: HERE are free links to my ebooks and best recent posts.
How to read this: Read it carefully if you or a loved one has AF. If not, read both parts of Jan’s story, then look at the rest of the essay for details about natural cures. Finally, read the ending about cardiology corruption.
Jan’s story, Part 1
She was 68 when she began having overwhelming exhaustion, and her electrocardiogram (EKG) showed on-and-off atrial fibrillation. Jan’s cardiologist prescribed medications, and her heart normalized for two years. However, when she developed pneumonia, she went into AF at 180 beats per minute and felt terrible.
She worked with the cardiologist for months, but although her rate was controlled, she stayed in atrial fibrillation. He finally shocked her heart (cardioversion), but it stopped for a prolonged period. He considered implanting a permanent pacemaker.
The cardiologist repeatedly adjusted her medicines, and another cardioversion put her heart into normal rhythm for a year, but her atrial fibrillation always returned (Continued at the end of the post).
Key basics
Atrial fibrillation is an irregular beating of the top of the heart (atrium) that causes the entire heart rhythm to become irregular. The rate is often uncomfortably rapid, but others have it and never find out until a doctor does an EKG. Short periods of AF may evolve into a continuous problem. Like most heart diseases, AF is usually a chronic problem that requires management but is rarely immediately dangerous. (Note: Ventricular fibrillation is immediately life-threatening and may occur after heart attacks.)
People with AF may have underlying lung or thyroid disease, high blood pressure, or other more severe issues such as heart failure or coronary disease. And although the symptoms are often minimal or moderate, AF can produce chest pain, heart palpitations, shortness of breath, and even loss of consciousness. Drugs, smoking, alcohol, and emotional stress sometimes play a role.
The big concern with atrial fibrillation is stroke. These happen when a blood clot forms in the irregularly beating atrium, then flips into the brain circulation. The downstream area’s blood flow is compromised, which may result in permanent damage or death.
AF can be suspected by an irregular pulse and confirmed with an electrocardiogram (EKG):
The upper recording is the irregular pattern of atrial fibrillation, and the lower one is a “normal sinus rhythm.”
In the normal heart of the lower tracing, “P” waves (lower arrow) arise from the atrial chamber at the heart’s top. The “wiring” in this area beats slowly and regularly to initiate each P wave and then heartbeat. The larger “QRS” waves after these are the electrical activity of the major heart chambers.
Although general internists and family practitioners treat atrial fibrillation, cardiologists see this problem daily and are the experts.
Beta-blockers such as metoprolol are typically used as the first treatment to slow the heart rate. They can sometimes “convert” the heart to a normal rhythm. However, other drugs and/or electrical shock(s) are sometimes necessary depending on the circumstances or in emergencies.
Some people are so treatment-resistant that the only therapy possible is to leave them in atrial fibrillation and reduce their heart rates to the normal 60 to 100 beats per minute. A few others have rates so low that they require electrical pacemakers.
(At one time, digoxin was used as the first-line drug, but its toxicity at relatively low doses has given the medical mainstream the idea that it is undesirable. Maybe this is also because it cannot be patented.)
Electrical burning or freezing of the heart’s wiring cells can be performed in an attempt to normalize the conduction defects causing abnormal rhythms. Although long-term results are debated, today’s techniques are more effective than those of a decade ago. This treatment may require an entire afternoon under anesthesia in the cardiac lab.
Anticoagulants, including aspirin and other low-grade anti-clotting agents like Plavix, are often used. For patients with heart disease or other factors that make strokes more likely, warfarin or the newer oral anticoagulants is standard practice. These reduce the yearly risk of stroke from a few percent to nearly zero but cause occasional serious bleeding. Warfarin works well but requires monthly blood testing, which leaves bruising.
AF affects about 2 to 3% of the population of Europe and North America. More recently, it has increased to 4% for the population between 60 and 70 years of age.
Astute AF patients know to get enough magnesium (MG)
Over half of all of us are magnesium deficient and should take it. MG should be used as part of the first-line therapy for hypertension and virtually every heart issue. It should be given intravenously to sick people as a routine, but few doctors do this even though it is harmless and effective.
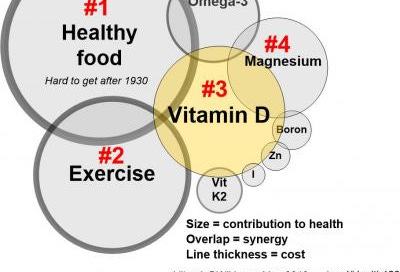
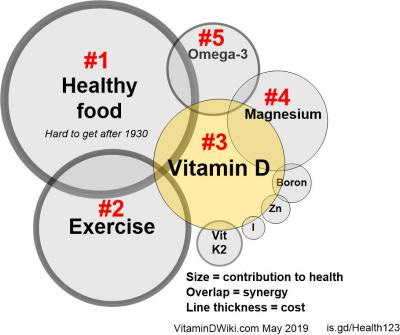
For perspective about MG, see the diagram below from Henry Lahore’s vitaminDwiki.com. Click the image to access more information.
Spend time on vitaminDWiki.com, subscribe to the Substack, and wave to Henry while you are there. The most important lesson he has is to be careful about diet; avoiding seed oils decreases inflammation, cardiac disease, and atrial fibrillation.
You should also look at my posts about boron, iodine, vitamin D, and, of course, magnesium. D levels* of 100 ng/ml improve health. Vitamin K2 (100 to 200 micrograms a day) and zinc (25 mg daily) are also critical for successful AF treatment.
*This blood test is available for $40 without a prescription at LifeExtension.com.
Key point: High vitamin D levels, perhaps 100 or even more, independently improve cardiac function and decrease your chances of AF. Study Henry’s references at the end of this post to convince yourself of this. If you have not discovered the 50,000 international unit D capsules, buy some online now. I take one almost every other day, and my levels are 130 ng/dl. Note: I am not recommending this to you and not giving medical advice. Read the references to decide.
CoQ is essential for anyone with heart issues or hypertension and independently improves MG absorption. Vitamin C is also necessary. Henry told me he would include this in the next version of his diagram.
These supplements work together, and each becomes critically important if you are deficient. Over half of us have critically low iodine levels, and many of my readers had profound health improvements when they took it. See my post HERE about that.
There are many types of oral magnesium, and they all raise blood levels but have different side effects and efficacy. The Costco brand containing 400 mg of magnesium oxide is great for constipation, but the glycinate form is better absorbed and helps your sleep and mood (Thorne is a reliable but expensive source).
Atrial fibrillation patients should keep their levels up by taking oral MG twice a day. There is no limit on how much can be consumed, except for loose stools.
Magnesium Type Uses & Notes
Magnesium citrate General, digestion, migraines, calm
Magnesium oxide. Laxative, very low systemic absorption. I like it.
Magnesium sulfate. Epsom salts. Muscle relaxation, calm
Magnesium chloride. Liquid/topical magnesium salt. Skin, calm, digestion, general.
Magnesium glycinate. Bioavailability, gastric health, muscle relaxation, mood, sleep, calm. I was told to take this.
Magnesium bis-glycinate. Good bioavailability, mood, sleep, nervous system, no laxative effect
Magnesium malate. Energizing, stimulates ATP production
Magnesium L-threonate. Brain health, nervous system, learning, concentration
Magnesium bicarbonate. Mixed in water to create a bubbly solution, good general magnesium
Magnesium taurate. Heart health, general calm, blood sugar regulation
Magnesium orotate. Heart health, general health
Magnesium aspartate Cellular energy, all around health
Pro-tip for blood pressure, cardiac, and AF patients: MG oil applied to the skin twice a day raises blood levels and might make prescription medications unnecessary for a few people. I recommend the Electra brand HERE (on Amazon HERE). Sandy, the owner, is my friend, and I interviewed her. If you mix DMSO (see my article about this) with MG oil, it will be better absorbed. See the Parting Shots for more.
Overdosing on magnesium is almost impossible, and several grams (not milligrams) is safe to give intravenously all at once, even to sick, hospitalized people.
Other medications
In an ideal world, magnesium would be the first consideration for atrial fibrillation and beta-blockers the second. Toprolol (metoprolol) is a long-acting brand that works well.
Beware: generic beta blockers often do not last 24 hours as advertised. Many people learn this the hard way when they have recurrent AF as the medicine wears off each day. Accepting a random pharmacy’s generic is a recipe for problems; the solution may be to pay extra for the higher-quality brand name.
Few patients realize that their doctors may be incentivized to prescribe cheap, lower-quality drugs that may not be as effective. See the Generics chapter of Butchered by “Healthcare” for a more comprehensive discussion. I show you there how to reliably and legally purchase economical brand-name drugs from outside the USA.
Calcium channel blockers such as diltiazem and verapamil are the next drugs of choice for atrial fibrillation after MG and beta blockers. These control the heart rate by slowing conduction through the heart's biological wiring.
Amiodarone is a powerful drug that consistently normalizes heart irregularities. It is often used in crises, especially if your doctor has to cardiovert (shock) you to restore normal rhythm. When I was in training forty-five years ago, its use was limited because of concerns about side effects. These include lung fibrosis, cataracts, dizziness, headache, chest pain, and many more. Nerve damage and numbness of the hands and feet can interfere with walking, and all these effects can be permanent.
Most people who take amiodarone are given it for three to six months, and side effects begin later, generally after a year. Most are given a high dose at first and then tapered down or off. The drug lasts many months in the body, even after you quit taking it.
Any blood pressure patient, cardiac patient, and almost everyone else should take magnesium. Newly diagnosed moderate hypertensives should routinely be placed on it before considering prescription medications.
Many have been sick for years and never learn they are magnesium deficient. Supplementation improves the heart, kidneys, blood pressure, and lowers heart rates. Those who are given amiodarone are often magnesium deficient. They should begin both the oral and topical forms immediately and think twice before taking amiodarone long-term. These situations are individual, of course, and your cardiologist will help.
Most blood pressure patients are given “non-loop” diuretics such as hydrochlorothiazide as their first drugs. I leave it to the reader to speculate why magnesium has been largely forgotten for this problem.
Omeprazole (Prilosec) is an acid-suppression drug sold by prescription and over the counter. Nearly everyone, with or without a medical license, passes it out like jelly beans. Prilosec blocks the effect of magnesium, which is terrible for everyone but particularly hazardous for those with AF because they may get breakthrough rhythm disturbances. When Prilosec is discontinued, atrial fibrillation sometimes vanishes.
Anyone sick, especially those admitted to the hospital, should receive intravenous supplementation with several grams of magnesium, five to seventy-five grams of vitamin C, at least 250 mg of hydrocortisone, and 250 mg of thiamine. When Pierre Kory proved that the last three saved lives, he lost his job as head of a major hospital’s intensive care unit.
Atrial fibrillation and blood thinners by the numbers
Those with AF have a three to four percent yearly chance of a stroke with brain damage. Blood thinners prevent this for all but a fraction of a percent but come with a small risk of bleeding into the brain or other parts of the body. Despite this, chronic blood thinner use is the best choice for most.
The older type, warfarin/Coumadin, requires monthly blood testing but is effective. The four newer ones, dabigatran, rivaroxaban, apixaban, and edoxaban, need no monitoring and also work well. Of these, the ones with fewer side effects are more expensive.
Temporarily stopping anticoagulants for five to seven days before surgery is standard practice and has few risks. A week off, for example, produces a stroke risk of (3 percent a year) divided by (52 weeks a year) equals .06 percent—.0006, six in a thousand. Your cardiologist can give you a more accurate idea of your situation, but it is guesswork even for him.
How Jan Conquered AF, Part 2
Since she is a registered nurse, Jan knows doctors and never believes anything they say on faith. Her husband is a physician, and she does not freaking listen (DFL) to him much, either—no man is a hero to his wife. She devised a natural program to help her body resist and prevent atrial fibrillation. Her goal was to get rid of some or all of her medications.
Jan always drinks a lot of water, but she started carefully measuring her fluids and now consumes an ounce per kilogram, 1/2 ounce per pound, every day. She is 150 pounds, so this is two liters. (I am 185 pounds, so this is 2.5 liters a day for me.)
Jan is hypertensive. Medical dogma says restricting salt controls blood pressure, but Dr. Brownstein encourages even his hypertensive patients to eat a teaspoon or more of yellow, unrefined Redmond or Celtic brand salt daily. This is successful. Jan might benefit because, like drinking more fluids, it would increase her blood volume and possibly make her heart function better. She knows that medical practice is largely folklore, but she is still “thinking on” using salt.
Jan’s research also uncovered Sandy’s magnesium oil, and she began slathering it on when she woke up and at bedtime. This creates reservoirs of the mineral in the skin that slowly release into the body. Since Jan has dry skin, she simply substituted the MG oil for some of the other creams she had been using. She also began taking oral magnesium twice a day and uses the oxalate alternated with the better-absorbed and calming glycinate.
Jan checked her vitamin D level and learned it was 125. Her doctor panicked, but she knew better from VitaminDWiki.com and ignored her. She also takes zinc, CoQ, vitamin C, and vitamin K2. She eats a lot of fish, so she rightly believes that iodine supplementation is unnecessary for her.
A careless doctor recently threw a prescription for Prilosec at Jan when she had a stomach upset. However, after Jan did her reading, she discovered that it blocks magnesium, so she trashed it. She never used alcohol or caffeine, so she did not have to quit these.
Jan read that higher magnesium levels improve women’s bladder control. This happened to her after she started topical magnesium.
Over a period of about two months, her vision began to fade, and she was forced to stop driving. Her opthalmologist diagnosed rapid-onset cataracts and sent her for surgery. She paid the extra $5000 for the fancy lenses that allow both close-up and distance vision and is very pleased with her “new eyes.”
Once she could see again, she began reading about her medications and learned that fast-developing cataracts were one of the many side effects of amiodarone. She had been on it for two years, but she immediately threw it in the trash and never took any more. (Note: I would ask the cardiologist’s advice before I would do that.)
Even though Jan quit many of her drugs, she has not had symptomatic atrial fibrillation for a year. She is now considering stopping her blood thinner, but I told her that if it were me, I would ask my doctor about that one.
NB: You likely know by now that this is not Jan but my wife, Judy. I added a few composite elements in Part #1 for illustrative purposes. As outlined in Judas Dentistry, her heart improved for other reasons during this period, so your results may vary using her program.
Judy is a skeptical animal, and this attitude has served her well. These days, it is survival itself.
References
Henry Lahore and VitaminDWiki.com’s info about the relationship between AF, vitamin D. and MG:
Atrial Fibrillation is DECREASED by Vitamin D or Magnesium - many studies and INCREASED by Calcium or high-dose Omega-3.
23+ VitaminDWiki pages with AFIB or FIBRILLATION in the title
5% less likely to get AFIB if ten ng higher Vitamin D - Maga-analysis Sept 2023
23% less likely for seniors to get AFIB if ten ng higher Vitamin D – 13 studies – 2019
Risk of Atrial Fibrillation Decreases if Vitamin D or Magnesium Increase - GRH Sept 2022
The Pathogenesis of Cardiac Arrhythmias in Vitamin D Deficiency - May 2022
Cardiovascular and Magnesium 17 studies
Cardiovascular and Calcium 14 studies
“Legal” disclaimer
You never read a Cliff Notes and thought the booklet was a doctor, did you? I am not your doctor, and this post is not your doctor, either. You must know your medical problems and medications well and carefully consider your care, but you should not treat AF without help from a cardiologist.
A few Cardiology Scams (excerpt from Butchered by “Healthcare”)
Heart doctors have their uses, but much of their work is expensive fraud supported only by faked studies. For example, the angioplasty procedures described below, with a few scant exceptions that I noted, are useless.
However you feel about cardiologists, be respectful and polite toward them. Like other doctors, they are mostly doing their best despite being tied up inside a box of lies.
The studies that debunked angioplasty and stents were unforeseen and staggering. In 2007, the NEJM published the “COURAGE” trial of over 2000 patients (study authors like acronyms; this one somehow stands for “Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation”). It showed that neither stents nor angioplasty improved survival or subsequent heart attack rates in patients with stable coronary artery disease.
A follow-up report by these COURAGE authors showed improvements in angina and a few quality of life measures, but these effects lasted less than 36 months. Based on this slender support, the operations continued. The cardiologists thought it was reasonable because stent deaths are so rare.
Finally, the ORBITA study showed conclusively that these procedures were without survival benefit for stable cardiac disease—for people who were not having a heart attack. Neither pain nor chances of further heart attacks decreased. This trial used an invasive “sham” or faked procedure for the control group, which is the most definitive type of surgical evaluation. There were only 230 patients, but the results were indisputable. (TheNNT.com has an excellent summary.)
Drug “eluting” stents leak drugs into the surrounding area, but they do not help patient survival either and cause an increase in blood clots. The science was clear: stents and angioplasty in routine care do not improve outcomes.
In 2019, a federally funded trial again discredited over 90 percent, possibly over 95 percent, of the cardiology and cardiac surgical invasive procedures. The researchers treated 5000 patients with stable heart disease with either CABG or stents. Neither therapy improved lifespan or heart attacks when compared to diet and drugs. These patients were not having heart attacks at the time of the interventions. The researchers also excluded those with left main coronary artery disease.
There is one narrow case where stents supposedly work. This is during a severe heart attack when the EKG has a pattern called “ST-elevation myocardial infarction” or STEMI. This is a complete or near-complete coronary artery blockage. When stents are placed during STEMIs, the cardiologists proclaim they save one person in 40, a number needed to treat of 40.
The American Heart Association and many others worldwide market this as “intervening during the golden hour” (lately, they have been promoting this more for strokes). Patients in their most vulnerable state, often in severe pain, get rushed from the emergency department to the catheterization lab and treated with angioplasty and stents. They are incapable of making reasoned decisions. Nortin Hadler summarizes: “Stenting belongs to one of the bleakest chapters in the history of Western medicine… Cardiologists are marching on because the interventional cardiology industry has a cash flow comparable to the GDP of many countries.”
The latest marketing ploy is to remind the public about “atypical” pain, which is serious but unlike the usual, distinctive heart attack pain patterns. People are now racing to the hospital, into this dysfunctional system, if they have any twinge in their chest.
Angioplasty causes strokes, heart attacks, rhythm disturbances, and bleeding. Does angioplasty save more STEMI patients’ during a heart attack than are killed by the procedure? When performed during a heart attack:
ANGIOPLASTY SAVES: 1/40, or 2.5%
ANGIOPLASTY FATALITIES: 1/167 to 1/43: .6% to 2.3%
ANGIOPLASTY COMPLICATIONS: 1/50, or 2%
Does the 1/40 “saved” figure already take into account the people who die from the procedure? Given the entire picture, I do not think it makes any difference, but if you still have doubts, ask your cardiologist. I doubt if they could convince me.
If we could forget the cardiologists’ conflict of interest and believe their numbers, the expense of doing angioplasties on 40 people to save one is 40 times the $35,000 cost, $1.4 million. This is on the outer fringes of acceptability; one to two million dollars spent for each life saved has somehow entered the literature as reasonable. Since heart attack patients have an average age in their late 60s, the number of years of life being bought is uncertain. And there are many other ways to spend this money that would do more good and save more years of life.
In the US, at least 85 percent (the lowest figure I could find) of coronary angioplasties are performed on patients who have uncomplicated, stable chest pain, where there is no chance of success. And STEMIs are likely only a percent or two of all heart attacks.
To justify the process, cardiologists often send their patients through the emergency room, claiming that they have “unstable angina.” This means chest pain occurring without physical exertion, not relieved by resting or medication, which may be worsening. This diagnosis gets abused since it is a judgment call with an imprecise definition. I spoke to emergency physicians in 2019, who confirmed they saw this scenario frequently.
Note: when angioplasty is done like this as an “elective procedure,” for no patient benefit, and not during a heart attack, it thankfully only kills .2 percent or 1/500.
Parting Shot #1
A reader sent me this about improving magnesium absorption using DMSO:
Trace Minerals Research is the cleanest magnesium I could find. You will experience a white residue on the skin that you can wipe off with a paper towel or washcloth. The white film is the chloride in the magnesium. It will not penetrate. Using this process, I was able to increase my serum magnesium levels.
Healing with DMSO by Amandha Vollmer is an excellent reference. She has recipes for eye drops, ear drops, and scalp spray, among many others. She says, “I have been using the eye drops and the scalp spray for a month or two now with no adverse reactions. It is too early to see if there are positive outcomes.”
Parting shot #2: for thirty years, captured sources have been running down coconut oil in favor of olive oil
Pritican: “The artery-clogging – and therefore most damaging – fatty acid is saturated fat. The fat in coconut oil is 92% saturated fat.”
Mayo Clinic: “Myth: Coconut oil is a heart-healthy cooking alternative.”
Harvard: “Because its cholesterol-raising effects were comparable to other saturated fats, [coconut] oil should not be viewed as a heart-healthy food and should be limited in the diet.”
If these “authorities” are against it, what more proof of its virtues do you need?
Coconut oil is almost magical. It is antifungal, antioxidant, and antimicrobial. “Oil pulling” after brushing improves oral health and kills plaque. I brush with it, then oil pull, and I hardly need to floss. It is 90 % saturated and has many other advantages described here.
Lineolic acid is the damaging polyunsaturated fat that accounts for almost 90% of PUFA intake in the US. Like macadamia oil, coconut oil is only 2 percent linoleic. Ghee is even lower, but olive oil, touted as the best, is 8.4 % linoleic.
Macadamia nut oil is 80% monounsaturated, 1% to 7% polyunsaturated, and the remaining 14% to 21% is saturated fat. It is great but not as good as ghee.









Share this post