He told me over dinner, “You are a Klonopin person, Robert.” My friend’s wealth always impressed me, and I assumed his patrician confidence reflected a matching erudition. I must have been conjuring the Yiddish proverb, “With money in your pocket, you are wise, and you are handsome, and you sing well, too.”
It was a time in my life when I blindly believed in Medicine, a time during which I became a heavy Prozac prescriber after reading Peter Kramer’s Listening to Prozac. It was decades before I learned my primary diagnosis was mercury toxicity from dental fillings. Like everyone else in medicine, Albert was treating symptoms rather than root causes.
I wrote about psychiatrists in Judas Dentistry:
Psychiatrists are drug pushers proffering elixirs that they claim cure a thousand ills. Sorry, I exaggerated. Only 450 “diagnoses” are found in their billing bible, the Diagnostic and Statistical Manual of Mental Disorders (DSM). To fabricate these, American Psychiatric Association members—paid handsomely by Pharma—cast votes. These “physicians” claim that “disclosing their financial conflicts of interests” fumigates this bribery.
The psych “diseases” concocted by these shills are expressly designed to be “treated” using pricey patented drugs. Pharma supplies half of the Food And Drug Administration (FDA) budget just as they pay the doctors, so their approval is a rubber stamp. Finally, massive disease-mongering campaigns run by corporate ad agencies convince us to use the purported remedies. Since the drugs are all highly addictive, little persuasion is needed after that.
This “mental health” industry has persuaded over a quarter of Americans (and 80 percent of Danes) to swallow psych drugs. Monthly shots are forced on others. These medications numb us, addict us, and cause violence, suicide, and social dysfunction. None has been proven effective.
The proof of that is that—just like every vaccine—the jackals running big Pharma never ran tests of their pricey nostrums against placebo controls. Studies lacking this vital metric are nonsensical. When the authors publish, they prove their work is a scam, the journal editors admit they are accessories, and the companies confess they are ringleaders in a racketeering conspiracy. The FDA blinds itself because it is paid off. All the people involved are murderers, for the drugs are killers.
Shrinks are trained like dancing bears to slap labels on people and medicate anyone coming within ten feet of them. Before he prescribed Klonipin, Albert sent me to one of his colleagues. This fellow was not at a loss for words, and his muddy torrent of them included an attempt to convince me that the Klonopin drug class (benzodiazepines) was more hazardous than SSRI “antidepressants.” At the end of our “session,” he tossed me a bag of colorful SSRIs that were in fashion at the time.
I tried them all, but each time, my body sensed brain damage. For more details about SSRIs, see their chapter from Butchered by “Healthcare, which I reproduced in the Parting Shots. It puts a flamethrower on these noxious pills.
And so I returned to Albert, and he taught me about benzodiazepines the hard way. He prescribed a hundred clonazepam with five refills and told me not to worry about addiction. I described this drug class in Butchered:
The benzodiazepines (Valium-class drugs) relieve anxiety for a few weeks. But after about a month, they stop working. After this, patients require higher dosages to produce the same effects. Later, if the drugs are discontinued, months of agonizing dread, sleeplessness, and crippling nervousness commonly occur.
The original studies of Xanax for anxiety were for 14 weeks; after four weeks, it was working; after eight weeks, it was not; and at the end of the study, as the experimenters withdrew the drug from the patients, they got much worse.
The psychiatrists and the drugmaker ignored the longer-term results and claimed a net benefit based on the first four weeks. (See Robert Whitaker’s YouTube.) The FDA approved the drug, and it became not only the most commonly prescribed benzodiazepine but the most frequently prescribed psychiatric medication. But Xanax is addictive, and most physicians are well aware of this by now.
Other benzodiazepines are also problematic to discontinue. Klonopin (clonazepam) is a chemically similar drug. One patient I worked with had used this 17-hour benzodiazepine to sleep every night for a decade. He decided to stop it, so I wrote a compounding pharmacy prescription for smaller and smaller doses that he took over three months. He suffered from anxiety and sleeplessness the whole time but felt better at the end. He said his energy and creativity both improved.
That patient was a composite that included me, and I became addicted for nine years. Since the drug’s effects last about eight hours, I would feel a little fuzzy but functional in the mornings. Those taking benzos tend to gradually increase their dose, and heavy Klonipen users take up to 8 mg or more every 24 hours and still crave it. I peaked and stabilized at two milligrams every night, which is considered an intermediate dose. Many combine the drug with drinking, but fortunately, in a life bedeviled with problems that included an alcoholic mother, this was never one of mine.
Last year, a surgeon friend who had read my book asked me for advice about quitting his clonazepam habit of twenty-some years. He had the same pattern as me.
It took months of sleepless nights, recurrent anxiety, and tapering doses for me to get off the damn stuff. A compounding pharmacist’s tapering doses can make this less painful and aggravating, but you must admit your problem to someone who might rat you out to the state medical board. So, I cut it down in stages. I was eventually able to convince myself that my free-floating withdrawal anxiety was unconnected to anything real, and I manned up for a few months and was done.
My final perspective after these experiences and my reading was that the benzodiazepines were horrible but benign compared to all other psych drugs. The SSRI antidepressants cause violence, suicide, brain damage, and far more severe addiction. The atypical antipsychotics have similar issues, plus they cut ten to twenty years off people’s lives.
In a rational world, no psych drug would have ever been approved. None have been adequately studied, and this is proof they do not work.
Another addiction
People compliment me on my smoky baritone podcast voice; a decade of cigarettes was how I acquired it. During my Klonopin period, I began smoking on a climbing trip at the encouragement of my buddy, Herb. Quitting these was more aggravating than stopping clonazepam. Herb is still puffing away.
The good news is that if ten or more years have gone by since you quit, your chances of dying of all causes are the same as people your age who have never smoked (reference). I am hoping for the best after this decade of foolishness.
My story is nothing
The following is excerpted from Christy Huff, M.D.’s website, benzoinfo.com. She went through a related addiction and withdrawal, but this article tells a more malignant story:
Christine Anne Narloch passed away on June 16, 2017, at the age of 48, after a long struggle with benzodiazepine withdrawal syndrome that ended in suicide…
In April 2015, she was prescribed 1mg of Ativan (lorazepam), which she took three times daily for symptoms of anxiety and tremors resulting from hyperthyroidism. She was not given informed consent at the time of prescription that the drug could cause physical dependence and severe side effects or that it was not intended for long-term use.
Initially, Ativan helped the symptoms for which it was prescribed, but after two months of taking it as prescribed, Christine developed a new cluster of symptoms… she was “now in tears most of the time and experiencing the inability to sleep and think properly, losing weight, having episodes of horrible fear and terror, burning nerves, episodes of severe pain, and thoughts of suicide.”…
She became unable to drive or care for her husband or her home. She visited multiple physicians who could not diagnose the cause of her symptoms… She became increasingly suicidal.
Knowing her life was at risk, she admitted herself to the hospital under the care of a psychiatrist, hoping that she would be helped. She was promptly diagnosed with a “nervous breakdown,” generalized anxiety disorder, and fibromyalgia. The psychiatrist decided to stop the Ativan abruptly, assuring the Narlochs that this was safe. What ensued during that hospital stay was not any relief, but instead a rapid onset of mental and physical torture that Christine would endure for the next 21 months…
Within a day of stopping Ativan, she had severe skin burning from head to toe. The next day, bright lights appeared before her eyes, combined with the feeling that her head was exploding, followed by a loss of consciousness for 30 minutes. When she awoke, she could barely walk for the next several hours, and the nursing staff ignored her pleas for help. She was released after six days in the hospital on a cocktail of risperidone, [an atypical antipsychotic] gabapentin, [a failed drug that was only approved originally for post-herpetic neuralgia], and hydroxyzine while still suffering horrific symptoms. Two days after discharge, she sought help again in the emergency room where the ER doctor diagnosed her symptoms as ‘benzodiazepine withdrawal,’ noting in her chart that she had not been tapered from the drug…
For the next 21 months, Christine continued to suffer. One of Christine’s most severe symptoms was akathisia, a state of inner restlessness with outer movement that compelled her to pace the house for hours on end. Mike was highly supportive and understanding of her situation, and he did all he could to help her. As a caregiver, it was difficult for him to feel so helpless, knowing that nothing could be done to make it better. Every day, he saw her forehead scrunch up as a wave of painful symptoms began. She would break out in a sweat, tremble, and cry. He remembers thinking how lonely and trapped she looked…
On the night she died, Christine sent a carefully worded letter… to a rarely-used email account. Her words make it clear that the relentless nature of the withdrawal symptoms led her to end her life.
Other references
I interviewed a woman who learned about SSRIs the same hard way that I learned about benzos. A shrink tossed her a prescription during a period when she was being ostracised by her Canadian family for refusing the vax. After a few days of use, she suffered akathisia with psychosis and was briefly hospitalized. She is an independent thinker, so she made the right choice and moved to Miami. The story is HERE.
My post about how SSRI antidepressant akathisia causes almost every mass shooting is HERE.
And HERE is my post about David Carmichael asphyxiating his young son in a hotel room while under the influence of an SSRI. The Canadian justice system eventually released him, and I met him and interviewed him. This is X-rated but required listening for students of reality.
MISSD, an akathisia awareness foundation, was started by my friend Wendy Dolan after her husband threw himself in front of a train two weeks after starting Paxil, an SSRI that is well-known for suicides. Her website is a great resource, and I am a donor.
#1 Parting shot: my psychiatrist Albert
He is a senior expert witness for the California workers’ compensation system, which wastes over half its revenues in administration. It is a network of senseless, expensive, prolonged litigation that primarily benefits lawyers and expert witnesses. Albert testifies about whether people have permanent psychological damage following industrial injuries. After 30 years of observing the scene from both the plaintiff (patient) and defense (state) sides, he says about half the plaintiffs are fakers.
He also reports that the insurance industry would rather spend more on litigation than recognize disability and fund timely care. Many cases are held up for years, which is disastrous to those with genuine health issues. Even though this delay runs up the ultimate cost of settlement, when the companies keep the money longer, they make more overall because they invest the withheld cash and get high returns.
Like the other players, Albert works the system. He has forty employees and contractors and bills the WC insurance companies at his lucrative physician’s rate for some of his employees' work. He claims this is a “grey area.” His income is $2 million a year, he works 20 hours a week, and he requested anonymity.
We are now out of touch.
The attached chapter from Butchered describes the workers’ compensation apparatus he works in. It is the second most corrupt healthcare delivery system. Download the following to learn the worst one:
Parting shot #2: Prozac and Relatives chapter from Butchered
I wrote about a thousand Prozac-type SSRI prescriptions over my career, which might have been a half-million dollars in drug sales. I screened my patients, as I was trained, by merely asking them a few questions.
Peter Kramer's bestselling Listening to Prozac (1997) duped me. He said Prozac could save patients from common symptoms of guilt, fatigue, sadness, sleep disturbance, and even aches or digestive problems. He also claimed it could be a lifestyle drug similar to today's Viagra, boosting ordinary peoples’ performance. I learned later that the SSRIs are toxic, have limited utility, and the hype has produced vast overuse.
Industry marketed SSRIs as an improvement on the older tricyclic antidepressants. These cause sedation, and only a month’s supply is needed for suicide. Part of the promotion of the Prozac-class drugs was that sleepiness is mild, and even enormous doses rarely cause fatality.
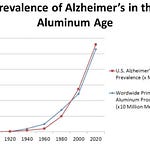
Before the drug era, doctors thought depression was rare and most often self-limited to about three months. Now (2020), Wikipedia claims that 17 percent of the US population becomes depressed during their lifetime, making them all candidates for expensive, indefinite medication usage. Legions of paid Wiki contributors, many of whom work for pharmaceutical companies, make this source only a little better than a drug industry link farm.
A simple checklist is used to diagnose depression. A primary care medical assistant often administrates it. It is a list of nonspecific symptoms from the DSM. Many are opposites.
DSM criteria for depression:
✪ Depressed mood most of the time
✪ Lack of pleasure most of the time
✪ Significant weight loss or gain, appetite up or down
✪ Slow or speeded-up thoughts and movements
✪ Feeling worthless or guilty most of the time
✪ Either fatigue or excess energy
✪ Cannot think or concentrate most of the time
✪ Thinking of death or suicide with or without a plan
No physical tests exist to verify the diagnosis. After waiting two weeks, doctors might commit a patient to these drugs for years—or even a lifetime. The industry promotes the disease, the medications, and the casual approach to treatment together.
“Prozac is not addictive,” according to the package label written by the manufacturer. True, there are no opioid-type withdrawals. However, after discontinuation, severe anxiety and depression are common. Other issues include suicide, feeling “electric shocks,” and tardive dyskinesia (TD), which is often manifest by continuous mouth movements. The drug companies claim most of this is because of the depressed state itself rather than medication effects. There were many consumer complaints to the Federal Trade Commission about these claims that antidepressants were not addictive.
When my patients sometimes stopped the SSRI drugs and had symptoms of depression and anxiety, I believed the propaganda that it was their disease and not the drug withdrawal. I was told that they must use the medications long-term for them to work, so I told everyone to continue. It was bogus information, however.
The Selective Serotonin Re-uptake Inhibitor (SSRI) name was pseudoscience dreamed up in the marketing department of SmithKline Beecham. The “chemical imbalance in the brain” idea was the brainstorm of a sales copywriter in the 1950s. Knowledge of serotonin and other neurotransmitters was even more sketchy when Prozac was invented than it is now. Today, this seductive but mythical gibberish embarrasses researchers.
Similarly, “ACE inhibitor” or “angiotensin-converting enzyme” blood pressure medications were gobbledegook names for branding. Lithium is an old therapy for bipolar illness with no sparkling, pseudo-scientific story associated with it. It is not patented or a money-maker, so no one will pay a copywriter to invent a marketing idea. Note: lithium causes sedation and occasional tardive dyskinesia. It becomes toxic in doses only slightly higher than the therapeutic ones. This can cause permanent brain damage.
The marketers said depression was like diabetes, and SSRIs were an “insulin” for brain disease. However, no clear relationship of depression to serotonin or other neurotransmitters was ever established, and the drugs all work about the same, with a similar lack of benefit. Jill Moncrieff in The Bitterest Pills (2013) confirmed this:
No chemical imbalance or other biological process that might explain drug action in a disease-centered way has been substantiated for any psychiatric disorder ... Most authorities now admit that there is no evidence that depression is associated with abnormalities of serotonin or noradrenaline, as used to be believed (Dubovsky et al., 2001). There is also little empirical support for the dopamine hypothesis of schizophrenia.
Ronald Pies, editor-in-chief emeritus of the Psychiatric Times, agreed: “The ‘chemical imbalance’ notion was always a kind of urban legend—never a theory seriously propounded by well-informed psychiatrists… [it was a] myth.”
Despite this consensus, nearly everyone still believes the metaphor and parrots the message. The idea is 1) your brain is damaged, 2) the drugs fix something, and 3) you need to take medications indefinitely.
SSRIs cause substantial harm. A 2017 literature review of randomized controlled trials in Frontiers in Psychiatry said these drugs are ineffective and damaging. It linked them to osteoporosis and movement disorders, including akathisia and tardive dyskinesia. They may double the risks of miscarriage and congenital disabilities. However, physicians use them off-label for pregnant women and during breastfeeding. Expectant mothers get severe withdrawal symptoms just like anyone else.
Sexual side effects occur in a range from 2% to 59% in various trials. In some studies, they never asked the patients about the issue. When used for premature ejaculation, about a third of men permanently improved, sometimes after just a few pills or even a single dose. This suggests significant long-term effects that are adverse for most people. Many patients report having long-lasting problems with having orgasms after taking and then stopping these drugs.
In the first nine years of Prozac's use, between 1988 and 1996, there were 39,000 FDA complaints, a record for any drug. This included reports of suicide, psychosis, abnormal thinking, and sexual dysfunction. Many patients taking the medication have sexual difficulties, are “emotionally numb,” and have “reduced positive feelings.” In October 2004, the FDA introduced a written warning about suicide in children and adolescents treated with SSRIs. The agency extended this in 2006 to include young adults up to 25.
Antidepressants are touted as preventing depression for people having medical problems. Prophylaxis is a market for nearly anyone.
Industry hid SSRI-related suicides and violence. The manufacturers have always claimed suicide was because of the underlying depression and not the drugs. They altogether avoided addressing violence, and the psychiatrists parroted this. Even Dr. Healy believed it before he worked as a plaintiff's expert in the Stewart Dolin case. So did I. Healy changed his mind after he read the secret corporate documents produced by the defendant corporation during the lawsuit’s discovery process.
Dr. Healy learned from his review that Lilly concealed suicides. Their executives had written internally that they could “go down the tubes if we lose Prozac” and that a single big news story could do it. In 1985, a Lilly internal memorandum said that the increased suicides were 5.6 times greater than those associated with imipramine, an older antidepressant. Gøtzsche later evaluated a 2006 FDA meta-analysis of 100,000 patients and estimated that it under-reported suicide by a factor of fifteen.
SSRIstories.org has thousands of news clips about SSRI violence. Martha Rosenberg summarizes:
The only thing more shocking than the number of newspaper stories on the site is the number of previously healthy people who committed violence with no precipitating events. Twenty people mentioned here set themselves on fire. Ten bit their victims (including a biter who was sleepwalking and a woman on Prozac who bit her eighty-seven-year-old mother into critical condition). Three men in their seventies and eighties attacked their wives with hammers. In Midwest City, Oklahoma, a woman accepted a cup of tea from an elderly nurse she'd just met—and then strangled her. A twelve-year-old boy left in his cousin's car while she shopped at Target killed her five-week-old daughter, who had also been left in the vehicle. All were under the influence of psychoactive drugs. Did events like these ever happen before the psychoactive drug revolution? In one month of reports on the site, a fifty-four-year-old respiratory patient with a breathing tube and an oxygen tank and no previous criminal record held up a bank in Mobile. An enraged man in Australia chased his mailman and threatened to cut his throat… for bringing him junk mail. A fifty-eight-year-old Amarillo man with no criminal history tried to abduct three people and killed an Oklahoma grandmother in the process. A sixty-year-old grandmother in Seattle killed three family members and herself. And fourteen parents drowned their children, a crime no one had heard of before…








Share this post