HERE is the Rumble video version of this post.
For new readers
Our health, finances, and political systems are being attacked. I cataloged more than 20 health assaults in my post, “Almost Everything Scares Me These Days”, and described the aggressors in the banker chapter of Cassandra’s Memo.
The worst healthcare disasters are vaccines, dentistry, and psychiatry, in that order. These cause even more havoc and death than oncology. Vaccines have increased the autism rate from 1/10,000 to one in thirty children—an incalculable future burden. Dental “care” is involved with 40 percent of first-world countries' diseases. Psychiatry has inflicted mortally damaging and totally ineffective drugs on a quarter of our populace. To learn about these calamities, read Judas Dentistry, Butchered by “Healthcare.”* and my vaccine posts (one is HERE); the final chapter of Judas Dentistry describes solutions. If you are unaware of all this evil, return to the links above when you can. (*Free download links.)
Today’s story is about life and hope.
Cures exist for even the most feared and common cancers—breast, prostate, pancreatic, and many others. Ms. Smith comprehensively describes the scene in her new film, A New Standard of Care: Alternative Cancer Therapies. It is free for now on YouTube—save the link.
If you, a friend, or someone in your family has cancer, stop what you are doing and watch this film. It has interviews with top alternative doctors and describes alternative cancer principles and effective treatments. It also uncovers those who oppose them. Pro tip: find the speed control in the lower right and turn it to 2x.
You can contact Megan Smith at msmithfilmmaker@gmail.com. Her other film is bOObs: The War on Women’s Breasts, an exposé of breast cancer screening. It won international film festival awards. Megan’s other links and references were unavailable at the time of this post’s publication, so we will put them in the comments.
An excellent related reference is Paul Marik’s Cancer Care and his interview HERE. He is the most published medical author alive and Pierre Kory’s brilliant partner at https://covid19criticalcare.com.
Failed Cancer Treatments
This chapter from Butchered by “Healthcare.” tells how oncology became a malignancy. Executive summary: only a handful of chemotherapies offer even a month of improved survival, and only a single disease, prostate cancer, is effectively treated by radiation. Butchered and this film tell complementary stories and should be studied together.
The patient is in the doctor’s hands. They will trust you to do anything at all. You must use good judgment and restraint.
Bill Cook, MD
Cancer is many diseases, and cures are elusive. Slow-growing tumors rarely require treatment because most never cause problems and may go away on their own. Fast-growing tumors are discovered too late to do anything. Only cancers of intermediate growth rate, a minority, have the potential for worthwhile intervention.
Chemotherapy improves survival for only a few tumors. These include metastatic melanoma, renal cell cancer, and a few lymphomas, leukemias, and testicular cancers. Tumor shrinkage and minuscule numbers prop up other treatments, but the expenses and toxicities make them failures.
Judging what is reasonable in this problematic field among these relatively weak remedies is challenging. Communicating the facts honestly and ethically with patients may be harder. Simultaneously, the physician must manage the emotions surrounding decline and death. This work requires a special person, and most doctors are not strong enough to do it.
Dying patients reach for anything. People with cancer are tremendously vulnerable and have an overwhelming need to trust caregivers. They continue to believe in their doctors, almost regardless of the circumstances. (How We Do Harm: A Doctor Breaks Ranks About Being Sick in America by Otis Brawley).
Oncologists always have new, toxic, and expensive drugs. They may have seen a few patients survive long-term using some medication that rarely works and makes everyone sick. They have read studies that showed (maybe) an average of two months of increased survival with certain drugs. They can usually tell the patient that a costly chemo might help and that it is covered by Medicare or insurance.
It is a demanding job, and the oncologists have a terrific financial conflict of interest that makes it harder. They retail chemotherapy infusions for about a 20 percent markup. Inside the specialty, they call this “buy and bill.” By 2013, 65 to 70 percent of oncologists' income was drug charges. Their pay doubled from 1995 to 2004 when it was $335,000, and then it went up again to $445,000 by 2017.
Drug representatives stay in touch with oncologists and tell them whether they are “making their quotas.” The companies offer doctors higher percentages for certain drugs if they order more. This is an inducement to raise the doses of drugs, which can be harmful. In one egregious case, medications were promoted in this fashion to treat anemia, but they also increased the chances of premature death. Their sales were $37 billion between 1996 and 2009. In How We Do Harm: A Doctor Breaks Ranks About Being Sick in America, Otis Brawley said, “[These] drugs were not used to cure disease or make patients feel better. They were used to make money for doctors and pharmaceutical companies at the expense of patients, insurance companies, and taxpayers.”
If two physicians made a deal like this between themselves, prosecutors might throw them in prison. “Fee-splitting” is a similar, perhaps nearly identical, crime where a physician kicks back a commission to another doctor for a patient referral. Federal Stark laws that apply to Medicare and Medicaid, plus many state laws, impose criminal penalties for this. (Between lawyers and between realtors, referral fees are accepted practice.)
Regardless of the legalities, our primary priority must always be our patients. These harmful and unethical incentives distract us from this duty and should be made illegal.
New chemotherapy medications can be 300 times (not 300 percent) more expensive than old ones. (See Deadly Medicines and Organised Crime: How Big Pharma Has Corrupted Healthcare by Peter Gotzsche). Cancer treatment expenses per patient are often over $100,000 a year. Jerome Kassirer adds:
One oncologist half-jokingly told me, "Chemo is our cardiac cath, or our arthroscopy," implying that chemo offers a profitable "procedure" for the oncologist [which is] "the dirty little secret of oncology." …Some oncologists… make an income of nearly a million dollars a year by pushing chemotherapy… approximately two-thirds of the income of oncologists in community practice was derived from intravenous or intramuscular drugs… [Quoting Dr. Eisenberg] "the financial conflicts I have identified in our discipline... are so pervasive and insidious that we continually must remind ourselves as to the real purpose of our work.”
On the Take: How Medicine's Complicity with Big Business Can Endanger Your Health (2004)
Gleevac, for example, is effective for some leukemias but costs nearly $9,000 for ninety 100 mg tablets. In 2014, we spent $92 billion on US cancer therapies, but in 2020, costs are projected to be $173 billion. Some treatments are hundreds of thousands of dollars a year for each person. Even patients who are near death get them. They experience the grim side effects for no benefit.
Only a scant few of the expensive, toxic cancer therapies improve lifespan. Once tumor spread has occurred, most chemotherapy barely helps. Drs. Graeme Morgan and his colleagues did an exhaustive literature search that was published in Clinical Oncology in 2004. They found that chemotherapy added only 2.1% to the 5-year survival for US adults treated for cancer. Nortin Hadler wrote in 2011 that survival has been extended only a few months for the most common tumors:
Lung cancers (except small cell): 2-6 months after several chemotherapies.
Breast cancers: drugs have not improved survival time. Early diagnosis has increased the number of cases, but death rates have changed little.
Colon cancers: from 9 to 22 months for the newest drugs.
Prostate cancers: 2 months.Rethinking Aging
He said this was a “dirty little secret” oncologists withhold from the public. There are new drugs every year, and many do not even improve the quality of life.
These opinions are dated, but Vinay Prasad, MD, evaluated the cancer drugs approved in 2016-2017. He wrote that they did not extend survival at all. He also studied oncology drugs that the FDA approved between 2008 and 2012. Thirty-six of the 54 were approved using surrogate endpoints and had no known effect on survival. Four years later, only five of them had been shown to help anyone live even a day longer. Prasad concluded that post-marketing studies should be required.
The American Society of Clinical Oncology knows all of this. Their 2014 goal for chemotherapy life extension was only 2.5 months. The 72 cancer therapies approved from 2002 to 2014 resulted in an average of only 2.1 more months of life than the older drugs. Only one in five from 2014 to 2016 worked even that well.
Otis Brawley, MD, agrees. He wrote: “I’m starting to hear more and more that we are better than I think we really are. We’re starting to believe our own bullshit.”
He said specialties that make money on diseases should not be deciding what is reasonable for testing or therapy. For example, radiologists should not be on panels deciding about the use of mammograms, and urologists should not determine radical prostatectomy standards. As obvious as this sounds, it is a radical idea for doctors.
Cancer ads make exaggerated claims about treatments that barely work. Although many therapies do not help people live longer, TV commercials typically promise “a chance for longer life.”
Dr. Prasad reviewed contemporary news stories for words like miracle, breakthrough, game-changer, and cure. Fifty percent of the time, they were used to describe drugs not approved by the FDA, and 14 percent of the time, they were talking about drugs that had only been tried in mice.
Timothy Turnham, former director of the Melanoma Research Foundation, an advocacy group, said, “There is a disconnect between what researchers think is statistically significant and what is significant for patients. Patients hear ‘progress,’ and they think that means they will be cured.” He was referring to chemotherapy approved for surrogate outcomes—a reduction of tumor size or some other result not affecting longevity.
Ad spending for cancer treatments has doubled in the five years ending in 2018. The total spent by cancer centers was $54 million in 2005 and $173 million by 2014. One group, Cancer Treatment Centers of America, did 60% of all the US cancer marketing that year.
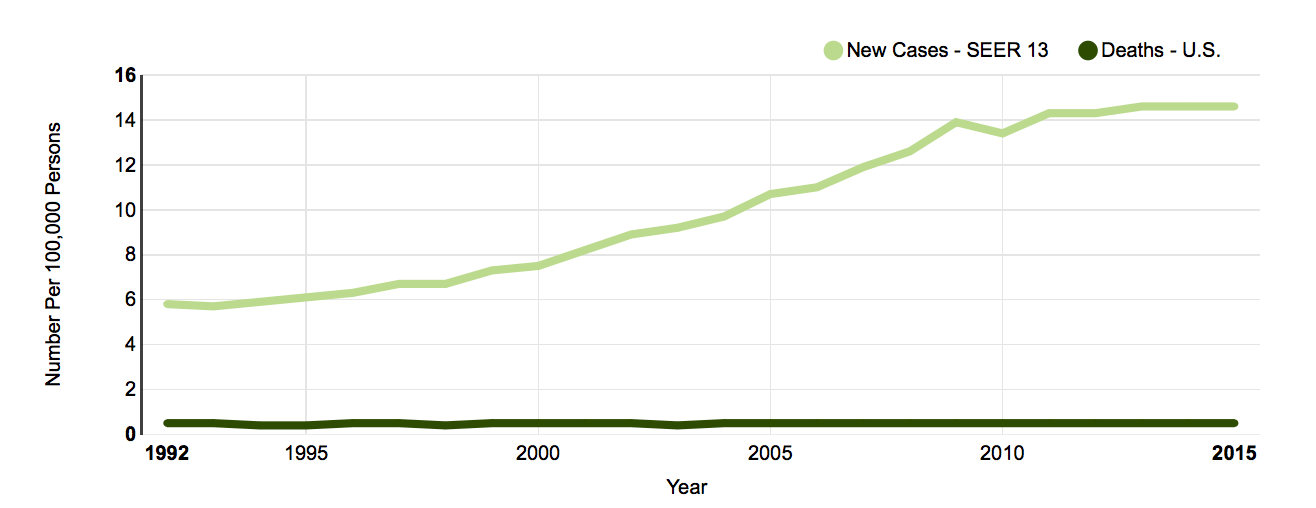
Another strategy is to frighten the public by telling them that the number of cancers is increasing. Most times, however, the fatality rate, which is the best measure of any cancer’s actual occurrence, has been unchanged for decades. Thyroid cancer, for example, is being discovered much more often, as seen in the top line of the graph below, but there has been no change in the death rate since 1992, which is the lower line1:
Thyroid cancer
One explanation could be that we are curing more cancers and saving more lives, but this is impossible—most of our treatments are ineffective or barely effective. These diseases are being discovered earlier and earlier by aggressive screening, which accounts for the increase in numbers. We promote anxiety, and we sell drugs. Most of the newly discovered tumors would go nowhere, even without treatment.
In South Korea, ultrasonic screening diagnosed 15,000 people with thyroid cancer, resulting in thousands of radical thyroidectomies, all of which required lifelong thyroid hormone replacement. The surgery caused vocal cord damage in two percent. However, mortality rates were rock-stable. This proves that this early diagnosis had no benefit and harmed some2.
Kidney cancer shows a similar pattern. Increases in diagnosis (top line) make the incidence seem to rise, but this has helped no patients. The cancer deaths (lower line) are the same year over year from 1992 to 20143.
Kidney cancer
Ineffective or barely effective cancer treatments are costing us a fortune. In 2014, US spending on oncology was $88 billion, and patients spent another $4 billion. Other estimates are closer to $100 billion now. The newest medications, often offering only a few months of progression-free survival, and not extending life at all, cost an average of $171,000 a year (2016). Some are $100,000 a dose (An American Sickness). As I published this book, the prices were still higher. They seem to reflect an attitude of “grab what you can.”
The industry mantra is that the newest is best, problems are a thing of the past, and that we must trust modern therapies. However, physician experience with many decades of new drugs debunks this. It takes years and thousands of patients before a medication can be deemed reliable. Failure or newly found toxicity is the most likely outcome with any novel treatment.
For example, the FDA approved a novel chemotherapy, the heavily hyped chimeric antigen receptor T-cell therapy. This uses genetically modified T white blood cells to kill cancer. The first drug in this class was approved in 2017, so long-term patient survival is unclear. It is mainly used for blood cancers, it sometimes has neurological side effects, and it may only work once. Then, the tumors recur. One estimate of the costs, including hospitalizations, is $1.5 million per patient.
Chemotherapy causes fatalities and dementia. For example, Avastin may produce a few months of survival advantage, or possibly the surrogate outcome of a few more months of disease-free survival. Unfortunately, when combined with certain other chemotherapy agents, it may make breast cancer patients die sooner. The FDA carelessly allowed it to be marketed for breast cancer in 2008, but three years later, follow-up studies showed heart attacks, bleeding episodes, and high blood pressure. The agency took the rare step of recalling it.
Even if patients survive, post-chemotherapy mental impairment or “chemo brain” affects 30 percent of everyone treated. This can include memory loss, visual changes, and even brain shrinkage. Tamoxifen, the anti-estrogen drug used for breast cancer, also causes mental impairment. Estrogen is vital to many human systems. Women need it to function at their best, and it is essential for men also.
THE SKIN CANCER CHARADE
I tried to become a dermatologist once. These specialists cleverly stay in their own world, avoid dealing with serious problems, and make a lot of money without losing sleep. It seemed like a masterful concept. I was an annoying young man, but through family connections and somehow conjuring a fragile veneer of charm, I got accepted into one of their most selective training programs. I thought this feat qualified me for the dermatologic lifestyle and wanted to spend my weekends hiking the Appalachian Trail. My mentors, however, thought I should spend 70 hours a week learning about skin diseases. After a year, they exposed me as a poseur and kicked me out.
I viewed it as a personal failure, but I smelled something fishy the whole time. I was too close to see clearly, and I had plenty of problems, so I could not put my finger on it. Like the dermatologists who were unsuccessfully trying to train me, I did not know the history.
The modern era for skin doctors started in the 1980s when the American Academy of Dermatology hatched a plan to contrive an epidemic of dangerous skin cancers. A Madison Avenue public relations firm charged them two million dollars to develop the idea. The proposal was for them to disease-monger themselves from foolish pimple poppers into fierce cancer fighters. After this, they evangelized about patients coming to their offices for a complete skin examination. This would supposedly prevent a plague of skin cancers. The USPSTF later exposed this idea as worthless and said the screening frenzy was promoting lucrative skin surgery rather than preventing cancer.
One ploy involved proclaiming the skin bumps they call actinic keratoses or AKs precancerous (dermatologists love names and acronyms). Many seniors have dozens, if not hundreds, of these. Since then, armies of skin doctors have been billing Medicare for treating millions of AKs with liquid nitrogen devices resembling tiny blow torches. Studies show that over half of all these bumps disappear on their own. Only one percent change to skin cancer after a year and four percent after four years, and these are virtually all slow-growing and easily treatable.
At about the same time, to handle this pandemic, dermatologists dreamed up the most expensive skin procedure ever seen, “Mohs” surgery. Many of these specialists bill Medicare hundreds of thousands of dollars a year for this alone. I have an acquaintance who does ten of these cases every Friday and gets paid about $15,000 each.
Patients spend up to a full day sitting around an accredited surgicenter operating room while dermatologists remove slices of their tumor bit by bit. They examine each morsel under the microscope as it comes off. A bill is submitted for each cut. There is another for processing each bit into a slide and yet another for each look into the microscope. This goes on until they have removed all diseased tissue.
After this, the area is “reconstructed.” This involves a lot of sewing, sometimes in areas as small as a dime. Insurance pays more if this is performed on a separate day, so the patient often gets sent home with a hole in their face. Sometimes, the patients get referred to plastic surgeons, who may use surgical center charges and other tricks to make even more money. In return, the plastics try to dig up skin cancer cases to send to dermatologists for Mohs treatment. These get bounced back to them for reconstruction.
At first, dermatologists did Mohs only for selected patients using careful criteria. Some body areas are critical for function and appearance, and their preservation can be essential. For example, this procedure produces excellent results for skin cancers of the nose and corners of the eyes. Other tumors have an octopus-like spread with indistinct borders. Here, Mohs is used to remove just the tumor with as little normal tissue as possible. These issues have all been worked out by dermatologists and published in their journals.
The older methods involved scratching, burning, or cutting away skin cancers. The holes were often left to heal without stitches, and we would then follow the patient for recurrence. Using a greasy antibiotic ointment a few times a day, normal healing regenerates the skin within a few weeks. The results are typically reasonable, even on the face.
Although this is adequate for the vast majority of skin cancers, dermatologists now perform Mohs indiscriminately. Robert Stern, a Harvard dermatologist, said, “The decision to utilize [Mohs] is likely to reflect the economic advantage to the provider rather than a substantial clinical advantage for the patient.” He reported wide variations in usage by the practice and region and estimated that the costs of Mohs surgery in the US were $2 billion in 2012. A panel that developed reimbursement criteria produced vague guidelines that justify almost anything. The experts making money made the rule—that they could do nearly anything they wanted.
Mohs is primarily used to remove basal cell or squamous cell skin cancers, which rarely leapfrog to other areas of the body. It is not appropriate for melanomas, which surgeons remove along with a sizable chunk of surrounding tissue to prevent these metastases. Mohs's primary advantage is that it reduces the chances of having to perform a second procedure for local recurrence. It also allows the surgeon to leave as much healthy tissue as possible.
The older, much less expensive method is to have the patient return a few months after cutting the skin cancer out to be sure there was no regrowth. This follow-up check takes only a few moments if no further work is necessary. Subsequent removal procedures are usually straightforward.
Mohs surgeries are medically minor procedures that require only local anesthesia. However, the fees are often higher than those for complex, lengthy, and hazardous general surgeries. Dermatologists spend money on lobbyists, who do their job defending exorbitant reimbursement for skin procedures.
Melanoma is the only skin cancer that routinely metastasizes and kills people. The dermatologists almost universally refer these cases to plastic surgeons for removal and then to oncologists for chemotherapy. Few skin doctors want to get involved with a fatal disease.
But when the dermatologists became cancer slayers, they began crying about the exploding numbers of melanomas along with the other skin tumors. As a result, they discovered so many that they claimed that melanomas were increasing faster than any other cancer. This epidemic now seems to be at the point of slaughtering anyone who dares to walk outside in the sunlight.
Left unsaid was that small, early tumors require only a simple procedure rather than an overpriced, supposedly complicated plastic surgery. Treating low-grade (thin) melanomas in seniors does not prolong their lives, either. However, once discovered, since progression into a fatal disease is unpredictable, they are cut off.
Because of all this, far more melanomas are being identified, but the total deaths are not increasing. Like thyroid and kidney cancer, the disease-specific mortality for melanoma has not gone up one iota (Worried Sick by Nortin Hadler). All the extra procedures to chase them, however, cost us time, pain, money, and anxiety.
The top line on the graph below is the number of tumors found. The lower line is the number of deaths, which is unchanged (National Cancer Institute).
Melanoma
A generous observer might say that the above analysis has not entered the dermatologic consciousness and that there are no wrongdoings here. But the specialty’s ringleaders understand it—they orchestrated the entire thing. And they made the story terrifying through disease-mongering.
People over 85 years old get twenty percent of all Mohs surgery. Many are performed in the last year of life and even the weeks before death. Demented people in nursing homes get frozen, biopsied, and operated on. These procedures hurt.
The skin doctors even got approval for a code to bill insurance for pimple-popping or “acne surgery.” During my training, when I reached a particular stage, they slapped the specially designed pimple extractor into my hand. I felt like a general surgery resident who was finally being given the scalpel to do my first appendectomy4.
CANCER TREATMENT CONCLUSION
Honest physicians place their patients’ interests ahead of their own. This does not always happen in cancer treatments. To an outsider like me, much of oncology seems like a toxic, expensive failure. Some of these treatments prey on people during their defenseless time at the end of their lives. But some work, some are cures, and a few are miracles. You have to do your research, make your decisions, take your chances, and stay hopeful. This field may be changing more rapidly than any other, and some of the outrageously expensive new drugs work.
Dermatologists self-promote and disease-monger. Most of the diseases they handle are cosmetic or nearly cosmetic.
Like the others, these specialties cannot resist reaching for all the insurance money stacked around them.
1 National Cancer Institute
2 Gilbert Welch, MD, described the debacle in the NEJM (2014).
3 National Cancer Institute
4 Much of this material came from dermatologist David Epstein’s online blog and a 2017 NY Times exposé of dermatology by Katie Hafner and Griffin Palmer.









Share this post